
This publication by Prato et al provides clinical evidence to the improved outcomes of using TAI in pediatric patients when coupled with an individualized approach upon initiation of TAI.
Introduction to the study
Transanal Irrigation (TAI) has been proven to be highly effective in treating children with continence issues due to organic causes such as previous colorectal surgery or neurological issues. One of the main limitations with the therapy has been the relatively high discontinuation rates. With this study, Prato et al looked to evaluate the efficacy of an advanced protocol for transanal irrigation tailored to each patient, with aim to prevent dropout and increase satisfaction, independence and quality of life.
Bowel problems in children
Bowel dysfunction, such as constipation and fecal incontinence occurs in up to 30% of children and adolescents and can be due to functional or organic disorders. The organic disorders can be further divided into neurogenic disorders (central nervous system disorders) or anatomical malformations that affect the spinal cord (spina bifida), as well as post-operative problems following surgery for Hirschsprung’s disease or anorectal malformations without any central nervous system or spinal cord involvement. Bowel problems in children are stressful both for the child and their caregivers and have been reported to lead to poor health-related quality of life and social problems, such as difficulty socializing with peers.
Does transanal irrigation help children with bowel dysfunction?
Transanal irrigation is a minimally invasive treatment for bowel dysfunction which uses a large volume of lukewarm water to irrigate the rectum and colon via the anus in order to initate peristalsis and expel stool. Regular use of TAI prevents bowel leakage and accelerates transit through the colon. With TAI the rectum and distal colon will be efficiently emptied of faeces and it takes approximately 2 days until new faeces reaches the rectum. The therapy is usually well tolerated and has low incidence of major side effects. Many previously published studies on the use of TAI in the pediatric population shows high rates of improvement in bowel function and health-related quality of life for both organic and functional conditions.
A personalized approach to TAI
Despite the positive results shown by previous studies, the use of TAI in the pediatric population is associated with high dropout rates reaching up to 30%. The dropout rates do however seem to improve with individualized training by qualified professionals. With this information in mind, Prato et al conducted this prospective, interventional, multicenter, nonrandomized study to evaluate the efficacy of an advanced protocol tailored to each patient or condition with the goal to prevent dropout.
The protocol began with patient recruitment (T-1) and within 8-weeks of recruitment the patients (and their caregivers) were trained in the use of a TAI device according to established practices (T0). During the T0 visit, the patients underwent a psychological and instrumental assessment which included a low-dosage barium enema with fluoroscopic assessment. The purpose of this assessment was to establish the exact amount of water needed for daily irrigation for each patient, which was done by determining the exact amount of diluted contrast needed to reach the splenic flexure of the colon.
The week following the T0 visit, the correct use of TAI and patients bowel function were addressed using Rintala and Visick scores (T1). Follow-up was then conducted face-to-face or by telephone at 8 weeks (T2) and 6 months (T3) after starting TAI.
How long does TAI take?
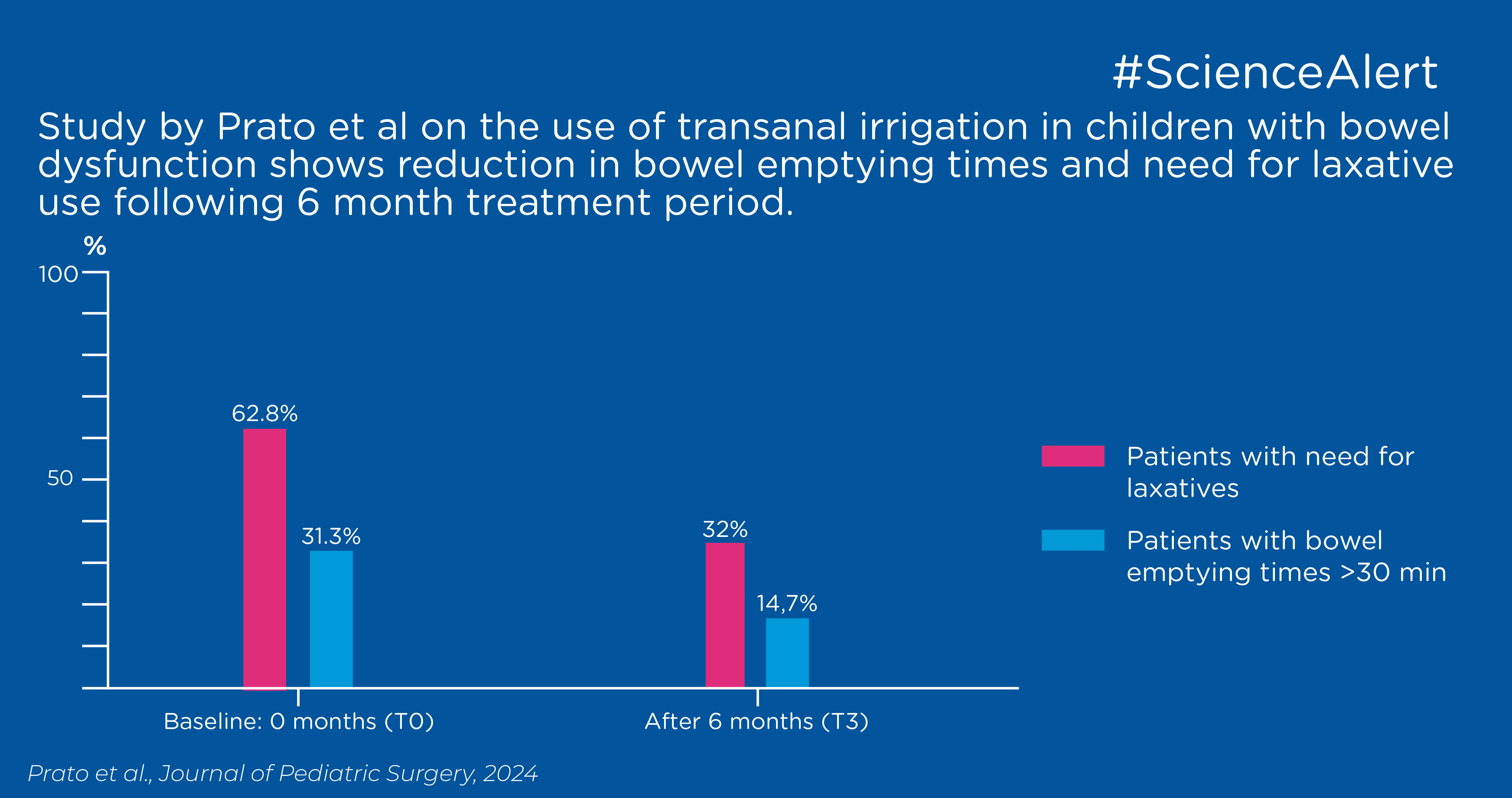
The study investigated bowel emptying times > 30min in the patients at T0 and T3. At T0, 31.3% of patients reported bowel emptying times >30min and at T3 the number had decreased to 14.7%. Similarly at baseline, 62.8% of patients reported the need for laxative use, while at T3 this number had decreased to 32%.
Using laxatives with TAI
Univariate analyses from the study showed that laxative use was a significant barrier to improvement, this was associated with a change in Visick grade and confirmed by multivariate analysis. The study showed that the patients who experienced the worst results following treatment with TAI were those with a regular laxative use and those who suffer from Spina Bifida (which proved to be an independent risk factor to poor outcome). The poor outcome following use of laxatives may be explained by the loosening effect of laxatives on stools and the difficulties diarrhea presents in regard to bowel management.
Urinary tract infections and TAI
At baseline (T0), 23.1% of the cases reported urinary tract infection. Following the use of TAI and getting a better bowel management routine in place, the number of reported cases significantly decreased to 2.6%, 5.3% and 8% at T1, T2 and T3 respectively.
Does the amount of water used for TAI matter?
The study observed that the higher initial volume of water used for TAI, the higher was the improvement of the Rintala score (as well as the other addressed scores). Therefore, the use of barium enemas at the first visit to establish the exact amount of fluid needed for the specific patient could be an impacting factor to ensuring effectiveness and patient satisfaction when initiating TAI.
While higher enema volume was associated with improvement, it was also associated with lower satisfaction in the univariate analysis, this was however not shown in the multivariate analysis.
Patient satisfaction with TAI
The goal with irrigation is to flush the stools out of the left colon to allow for a period free from accidents, preventing leakage between irrigations. The study could observe an improvement in satisfaction reported by parents/caregivers. The percentage of subjects reporting a grade 1 Visick score almost doubled between T1 and T3 (from 48.1% to 82.7%) while the percentage of patients reporting all other levels of the Visick score significantly decreased.
During the study period, an increase in the scores was observed to be consistent to what has been shown in other studies at 6- to 14-month follow-up. Fair to poor continence significantly decreased during the treatment period, with less than 15% complaining of major continence issues at the end of the study period (after 6-moths continuous use of TAI).
Other parameters and outcome measures, including pain and bleeding during defecation and sensation of incomplete emptying, dramatically improved during the study period as well.
Summary
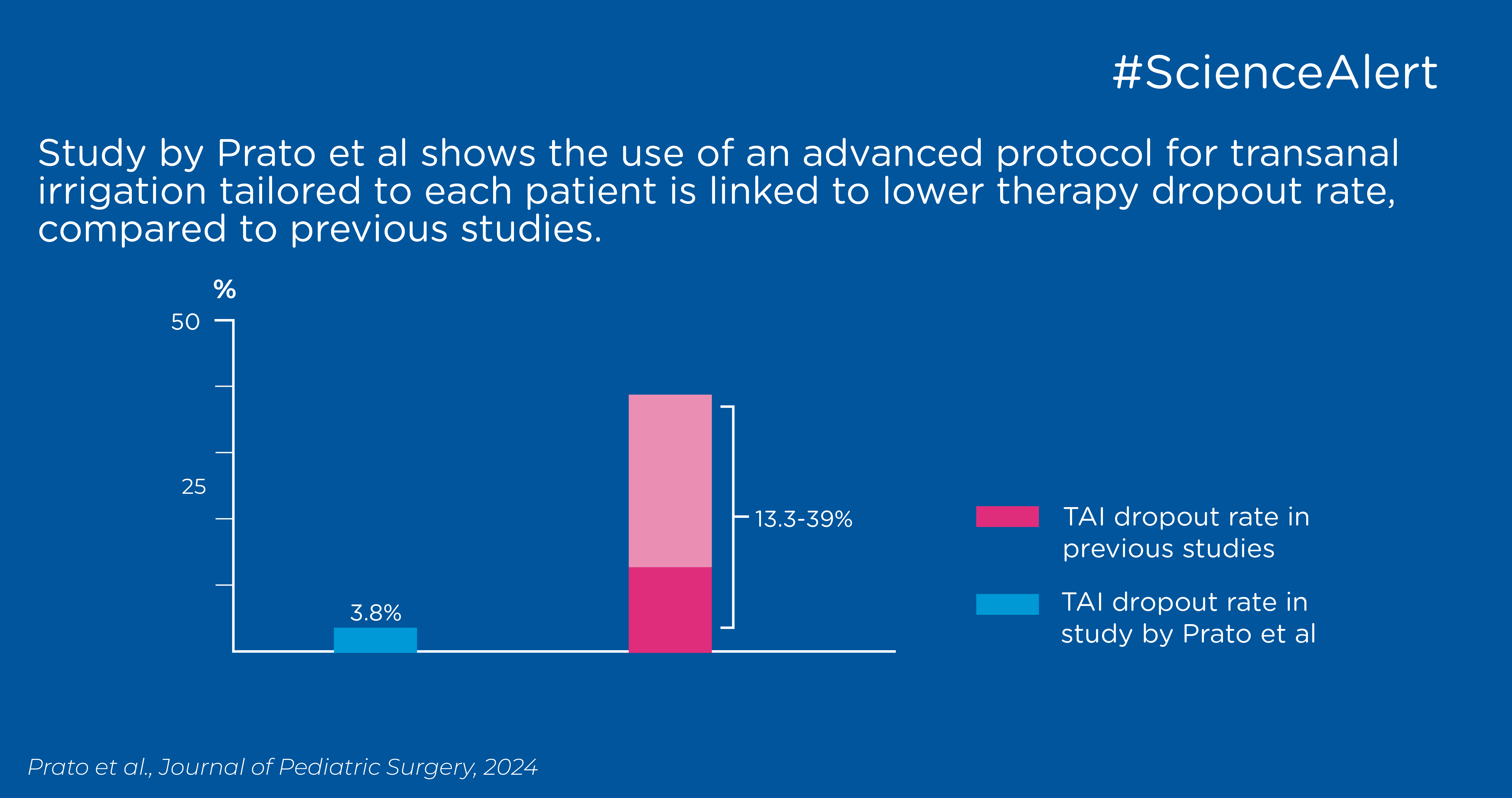
Overall, the study confirms that TAI is a successful treatment for children with organic bowel dysfunction who do not respond to conservative treatments, regardless of the underlying cause of symptoms. The study also shows that with an individualized approach to the initiation of TAI, their dropout rate was measured at 3.8%, which is significantly lower than the results of previous studies which range from 13.3% to 39%. One could therefore speculate that the tailored indication for water volume using barium enemas during TAI administration represents the most significant improvement and peculiarity of the study's proposed methodology.